
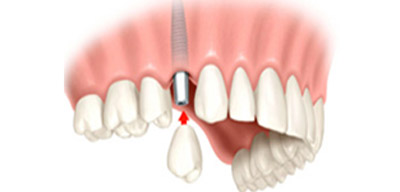
A dental implant is a surgical component that interfaces with the bone of the jaw or skull to support a dental prosthesis such as a crown, bridge, denture, facial prosthesis or to act as an orthodontic anchor. The basis for modern dental implants is a biologic process called osseointegration where materials, such as titanium, form an intimate bond to bone. The implant fixture is first placed, so that it is likely to osseointegrate, then a dental prosthetic is added.
It is important that you are in good health, however, as there are some conditions and diseases that can affect whether dental implants are right for you. For example, uncontrolled diabetes, cancer, radiation to the jaws, smoking, alcoholism, or uncontrolled periodontal (gum) disease may affect whether dental implants will fuse to your bone. It is important to let your dental surgeon know all about your medical status (past and present) together with all medications you are taking, whether prescribed, alternative (herbal) or over-the-counter. Where and how implants are placed requires a detailed assessment of your overall stomato-gnathic system (“stoma” – mouth; “gnathic” – jaws), within which the teeth function. This will necessitate compiling records that include study models of your mouth and bite, and specialized radiographs (x-rays), which may include 3D scans known as computerized tomograms (CT scans). Planning with the help of computer imaging ensures that dental implants can be placed in exactly the right position in the bone.
Immediately (at the same time an implant is placed) or after a period of healing, an abutment is attached to the implant. This is a device that “abuts” or joins the implant to a tooth form called a crown, which replaces the tooth part you see in the mouth. It will hold a custom-made crown that the dental laboratory will fabricate and match to your existing teeth. The custom crown is cemented or screwed onto the abutment to permanently keep it in place. Once the crown is in place, it should be indistinguishable from your natural teeth.

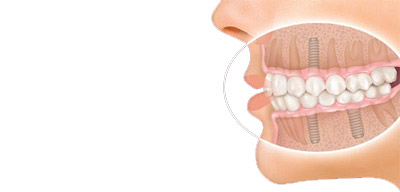
As with single tooth replacement, temporary healing caps or abutments may be placed on multiple implants until the healing phase is complete. After healing, permanent abutments are attached to the implants. They can attach to custom-made crowns or bridgework that a dental laboratory will fabricate to match your existing teeth. In the final step, the custom bridge, which will replace multiple teeth, is cemented or screwed onto the abutments. The teeth have been replaced without disturbing the healthy teeth next to them, and bone loss has been halted.
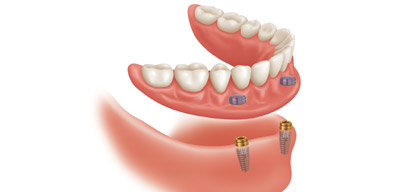
If all of your lower teeth are missing, depending on the design of the removable restoration, two to six implants may be used to support a lower denture. If all of your upper teeth are missing, a minimum of four implants may be used to support an upper denture. Removable dentures are often used to replace extensive tooth, bone and gum-tissue loss, thus providing support for the facial skeleton, lip and cheeks. A new denture can have attachments that snap or clip it into place on the implants or a custom made, milled bar can be fabricated to create additional strength and support for the restoration. Design variations are often related to your bone density and number of implants present; your dentist will discuss these options during your consultation. A significant advantage of a removable denture is facilitating the cleaning of the dental implants.
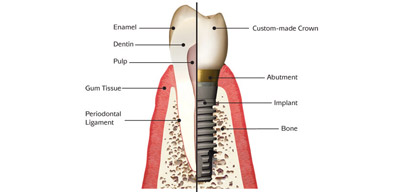
Natural teeth and dental implants may look the same, feel the same, and even function in a similar way, but they are very different. The most important differences are in the way they attach to the surrounding bone, their response to dental disease, their maintenance, and repair.
Teeth attach to the surrounding bone by a periodontal ligament (“peri” – around; “dont” – tooth) made up of collagen fibers that join into the tooth on one side and bone on the other. Dental implants fuse directly to the bone.
The gum tissues also attach to the root of a tooth with collagen fibers as described above. However, gum tissues can only stick to the surface of dental implants.
Teeth are susceptible to dental decay as well as the need for root canal therapy; dental implants are metal and do not decay or need root canal. Teeth may also be susceptible to periodontal (gum) disease, while dental implants may be susceptible to peri-implantitis, an inflammatory response to bacterial biofilm of the tissues surrounding the implant, which can result in disintegration of the bone to the implant.
Implant crowns and other prosthetic (false) tooth replacements are made to be remarkably failsafe systems. They are removable and replaceable (only by your dentist), so that if damage or wear necessitates replacement, this can be accomplished without affecting the implant(s) or attachment to the bone.
Nevertheless, implants do require maintenance. It is important to practice good daily oral hygiene, including brushing and flossing to control bacterial biofilm. It is also important to see your dentist and dental hygienist. Special instruments are necessary to clean dental implants that will not damage their metal surface beneath the gum tissues. Your dentist will need to monitor your implants to make sure the integrity of the osseointegration is stable, and that the implant crowns, bridgework or dentures are functioning adequately.
Bone needs stimulation to maintain its form and density. In the case of alveolar (sac-like) bone that surrounds and supports teeth, the necessary stimulation comes from the teeth themselves. When a tooth is lost, the lack of stimulation causes loss of alveolar bone. There is a 25% decrease in width of bone during the first year after tooth loss and an overall decrease in height over the next few years.
The more teeth lost, the more function lost. This leads to some particularly serious aesthetic and functional problems, particularly in people who have lost all of their teeth. And it doesn’t stop there. After alveolar bone is lost, the bone beneath it, basal bone — the jawbone proper — also begins to resorb (melt away).
It takes a dental team to assess and plan dental implant placement and restoration — the fabrication of the crowns, bridgework or dentures that attach atop the implants and are visible in your mouth. The dental team consists of a dental surgical specialist — a periodontist, oral surgeon, or a general dentist with advanced training in implant surgery; a restorative dentist, who plans and places the tooth restorations; and a dental laboratory technician who fabricates them.
Placing dental implants requires a surgical procedure in which precision channels are created in the jawbone, often using a surgical guide. The implants are then fitted into the sites so that they are in intimate contact with the bone. They generally require two to six months to fuse to the bone before they can have tooth restorations attached to them to complete the process.
Grafting bone into the extraction sockets at the time of tooth loss or removal can help preserve bone volume needed for implant placement. Surgical techniques are also available to regenerate (re-grow) bone that has been lost, to provide the necessary bone substance for anchoring implants. In fact, a primary reason to consider dental implants to replace missing teeth is the maintenance of jawbone.
Bone needs stimulation to stay healthy. Because dental implants fuse to the bone, they stabilize it and prevent further bone loss. Resorption is a normal and inevitable process in which bone is lost when it is no longer supporting or connected to teeth. Only dental implants can stop this process and preserve the bone.

A broken jaw is a common facial injury. Only the nose is broken more frequently. A broken jaw is the 10th most common fractured bone in the human body. Fractures (breaks in the bone) are generally the result of a direct force or trauma to the jawbone (mandible). A dislocated jawbone means that the temporomandibular joint (where the jaw connects with the skull) is moved out of place. The jawbone may or may not be fractured, but even if there is no fracture, symptoms (listed below) may be similar to a jawbone fracture.

An oral and maxillofacial surgeon or your dentist can remove (extract) a wisdom tooth. The procedure often can be done in the dentist's or surgeon's office. You may have the surgery in the hospital, especially if you are having all your wisdom teeth pulled at one time or if you are at high risk for complications. If you have any infections, surgery will usually be delayed until the infection has cleared up. Your doctor or dentist may have you take antibiotics to help heal the infection.

Oral and maxillofacial surgeons at our clinic evaluate, diagnose and treat the full spectrum of cysts and tumors in and around the jaw and structures of the teeth. These include benign tumors and cysts, which are non-cancerous; those that are aggressive and growing, with the potential to become cancerous; and tumors that are malignant, meaning that they are cancerous. Our oral and maxillofacial surgeons also treat oral cancer, severe infections of the oral cavity, salivary glands, jaw and neck.

Its a common misconception that cosmetic surgery always involves use of artificial material, its a big confusion, cosmetic surgery is surgery which is intended to improve your look when functional problem is not there, in fact almost every cosmetic surgery involves improvement of both look and function & every effort is made to achieve it by remodeling your own body tissue, rather than using allo-plastic ( Artificial ) material (unless essential),best example you may see in Rhinoplasty.
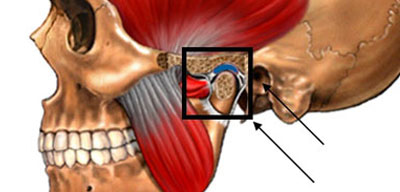
Temporomandibular joint and muscle disorders (TMJ disorders) are problems that affect the chewing muscles and joints that connect your lower jaw to your skull. There are two matching temporomandibular joints on each side of your head. They are located just in front of your ears. The abbreviation "TMJ" refers to the name of the joint but is often used to mean any disorders or symptoms of this region.

The treatment of patients with oral submucous fibrosis depends on the degree of clinical involvement. If the disease is detected at a very early stage, cessation of the habit is sufficient. Most patients with oral submucous fibrosis present with moderate-to-severe disease. Moderate-to-severe oral submucous fibrosis is irreversible. Medical treatment is symptomatic and predominantly aimed at improving mouth movements.

Orthognathic surgery is surgery to correct conditions of the jaw and face related to structure, growth, sleep apnea, TMJ disorders, malocclusion problems owing to skeletal disharmonies, or other orthodontic problems that cannot be easily treated with braces. Originally coined by Harold Hargis, it is also used in treatment of congenital conditions like cleft palate. Bones can be cut and re-aligned, then held in place with either screws or plates.
Reconstructive surgery is, in its broadest sense, the use of surgery to restore the form and function of the body; maxillo-facial surgeons, plastic surgeons and otolaryngologists do reconstructive surgery on faces after trauma and to reconstruct the head and neck after cancer. This ranges from very simple techniques such as primary closure and dressings to more complex skin grafts, tissue expansion and free flaps.